Abstract
Introduction
Aplastic anemia (AA) is an immune mediated bone marrow failure syndrome characterized by reduced numbers and dysfunctional regulatory T cells (Tregs). Using deep phenotyping, we have previously identified an immune signature that predicts clinical response to immunosuppression (IST) (Kordasti et al., Blood 2016). The so-called Treg A (CD4+CD25hiCD127loCD45RAhiCD95-CCR4lo) were higher in IST non-responders, whereas responder patients had a higher proportion of Treg B (CD4+CD25hiCD127loCD45RAloCD95+CCR4hi). The aims of the current study were to investigate the reasons for the reduction of specific Treg subset, the ex vivo expandability of the remaining Tregs in response to IL-2, their function and stability following expansion. The efficacy and longevity of these cells were tested in an animal model, with the aim of using autologous ex vivo expanded Tregs as a potential treatment for AA.
Methods and Results
FAS-L-induced apoptosis leads to reduction of Treg B, this effect can be reduced by low-dose IL-2
Given the role of FAS-L positive T cells in the pathophysiology of AA pathophysiology and the fact that CD95 (FAS) is one of the significant non-redundant markers that defines Treg B, we tested the FAS-L sensitivity of these cells. After 5 hours culture with FAS-L (5 mg/ml), the number of apoptotic cells was significantly higher in Treg B compared to Treg A (3 replicates, p < 0.02). The effect was prevented by the addition of low-dose IL-2 (5 U/mL) to the culture.
Treg expansion and their function
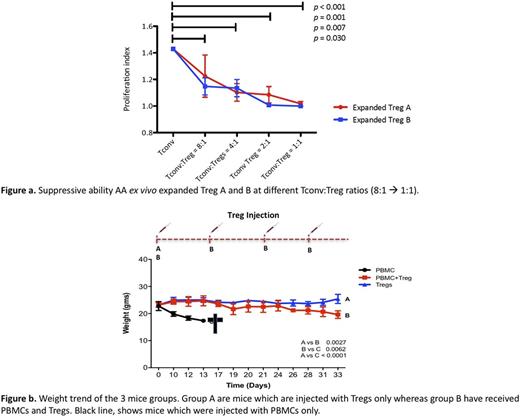
Total Tregs from AA and healthy donors (HDs) are sensitive to low dose IL-2 as shown by STAT5 phosphorylation (p < 0.001, n = 6 AA and 2 HDs). Moreover, Tregs from AA and HDs can be expanded polyclonally at a comparable rate (fold increase 33x vs 21x, p = n.s. n = 6 AA and 8 HDs) in a Treg promoting culture (stimulation with anti CD3/CD28 beads and IL-2 1,000 IU/ml for 4 weeks with all-trans retinoic acid and rapamycin). Although Treg A had lower level of p-STAT5 in the presence of low-dose IL-2, this reached to a similar level to Treg B following culture with higher doses of IL-2. To investigate the potential differences between Treg A and B in terms of function and expandability, Treg A and B were sorted from 6 HDs and 4 AA patients, and then expanded for 4 weeks (as above). Treg A and B expanded in HDs (Treg A 45x, and B 33x fold increase, p = n.s.), whereas Treg A expanded at a higher rate compared to Treg B in AA (Treg A 2120x, and B 90x fold increase, p = 0.03). The in vitro expanded Treg A and B both suppress proliferation of conventional T cells (Tconv) (n = 6, p < 0.001, no difference between A and B, figure a). Treg stability was assessed by DNA methylation analysis using deep amplicon bisulfite sequencing of the Treg-specific demethylated region (TSDR) . TSDR CpG sites in the expanded Treg A and Treg B populations from HD and AA patients are 2% and 13% methylated respectively, confirming their stability.
Treg function in vivo
To test the suppressive ability of these Tregs, we transplanted NSG-SGM3 mice with either HDs PBMCs alone (n = 3), or HDs ex vivo expanded Tregs alone (n = 3) or HDs PBMCs co-injected with HDs ex vivo expanded Tregs (n = 3). Mice injected with both PBMCs and Tregs received a further dose of Tregs at day 16 and then weekly injections until day 28. Mice injected with PBMCs only had worst overall survival compared to the mice with PBMCs + Tregs or Tregs only (13 versus 35 days, p < 0.0001) and developed acute GVHD during the first 10 days following the injection (day 13 PBMCs mice 17.36 g versus PBMCs + Tregs mice 22.7 g, p = 0.0052, figure b). There was no weight difference between PBCs + Tregs mice and Tregs only mice.
Conclusions
In summary, although the FAS-L sensitive Tregs, which are the most functional Tregs, are reduced in AA, the remaining Tregs in these patients are IL-2 responsive and can be expanded in vitro . We were able to sort Treg subpopulations (Treg A and B) from AA patients and show that they are expandable, stable and functional up to 8:1 ratio with Tconv. We have also tested the efficacy of ex vivo expanded Tregs in preventing GVHD in a mouse model. Overall, the current study suggests that in AA there may be an increased exposure to FAS-L and an insufficient level of IL-2, which selectively induce apoptosis of Treg B. Moreover, the ex vivo expansion of stable and functional AA Treg subsets is feasible. The expanded Tregs are likely to be able to control the inflammatory response in these patients, hence pave the way toward a novel cellular therapy for AA.
Kordasti: Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal